



To receive important alerts and updates from Gold Coast Primary Health Network, please submit the form below.
"*" indicates required fields

To receive important alerts and updates from Gold Coast Primary Health Network, please submit the form below.
See pdf version here.
We continue to have an instrumental role during the COVID-19 response through crucial engagement and information to health professionals and the community, supporting the vaccination program for GP practices and aged care facilities, vulnerable groups and Commonwealth funded general practice respiratory clinics (GPRCs), distribution of personal protective equipment and promoting vaccination to improve uptake, through engagement and communication campaigns.

read more

We have been involved in supporting the vaccination of vulnerable populations including people who are homebound, homeless, have mental health/substance abuse issues, people of non-English speaking backgrounds and the Aboriginal and Torres Strait Islander community. This has been through supporting in-home vaccination services, group and mobile vaccination clinics and widespread education and promotion, to encourage uptake of the COVID-19 vaccination. Our work has included:

We would like to acknowledge the significant collaboration with our partners and stakeholders in the continued COVID-19 response.
|
|
read less
The Joint Regional Plan (JRP) for Mental Health, Suicide Prevention and Alcohol and Other Drugs (AOD) was launched in 2020 as a joint initiative with Gold Coast Primary Health Network (GCPHN) and Gold Coast Health (GCH) in collaboration with clinicians, service providers and people with a lived experience.
The plan is a roadmap for our shared activities which align with regional strategic needs and priorities, to ensure people can live life with meaning and purpose within a compassionate, connected and diverse community.
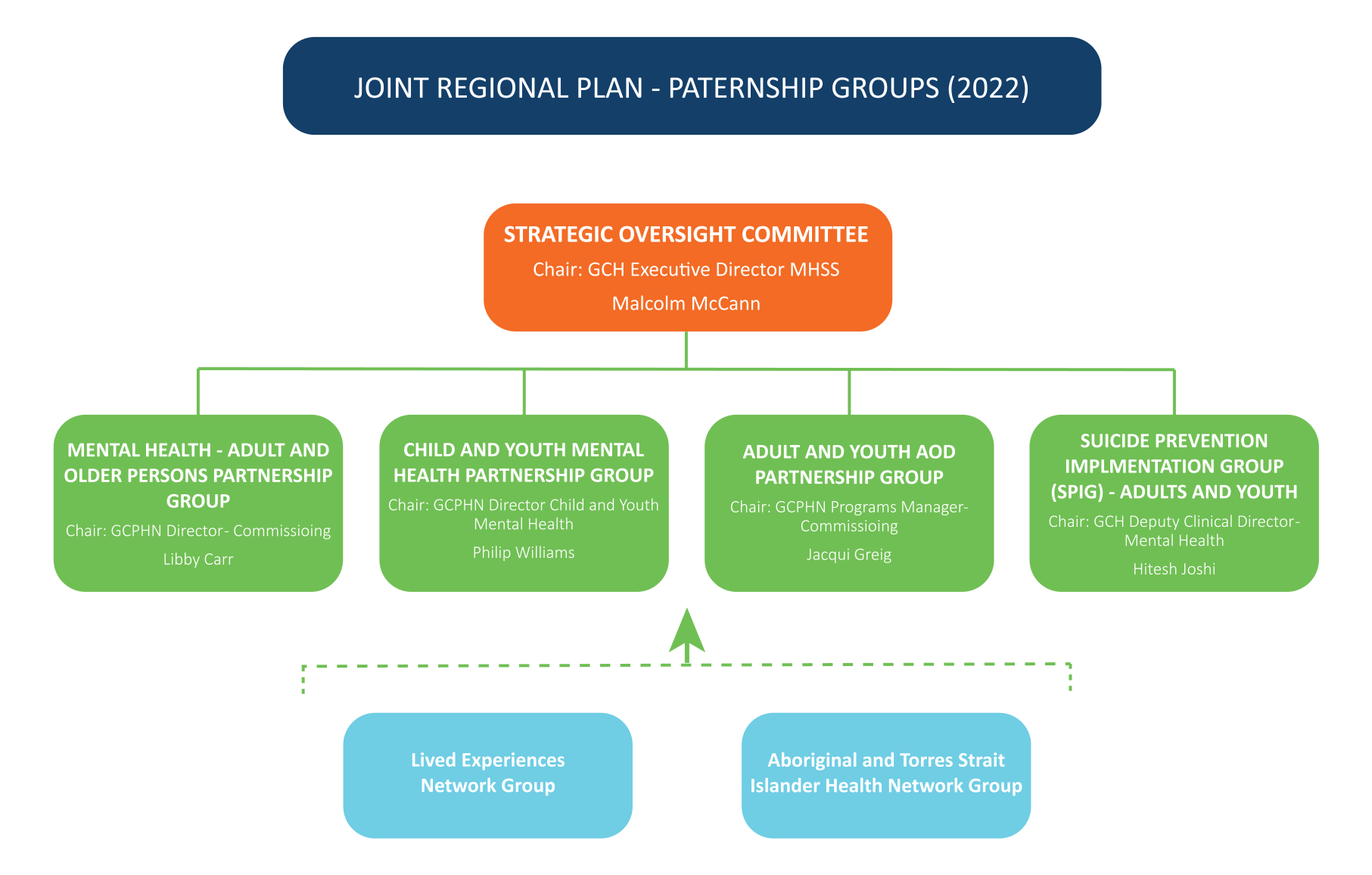
To support the implementation of the Joint Regional Plan, partnership groups have been established bringing together service providers, individuals with lived experience and key stakeholders who report to the Strategic Oversight Committee. Their combined knowledge will help to consider needs from within the plan to assist people living with severe and complex mental health, alcohol and drug concerns and support suicide prevention.
In the last 12 months the following has being achieved under against the key focus areas of the Joint Regional Plan.
read more
Leadership, governance and partnership, including lived experience
Planning for a common agenda
Coordinated activities that leverage and enhance strengths
Responsive and connected workforce
Effective, timely and safe information exchange
read less

The Suicide Prevention Implementation Group (SPIG) was established in 2022 as one of the Joint Regional Plan partnership groups. This group was established to progress the Suicide Prevention Community Action Plan which was launched in 2021, developed by Gold Coast Primary Health Network (GCPHN) and Gold Coast Health (GCH) with support from networks, community groups and individuals with a lived experience. This plan, together with the SPIG, strengthen relationships and collaboration in the planning, coordination and implementation of suicide prevention activities for the Gold Coast. It is intended to foster supportive social relationships, encourage effective help seeking and positive connections of health services, and support family harmony and a sense of purpose and control.
“Suicide prevention requires a whole of community approach in designing, delivering and coordinating efforts across the region and the Community Action Plan sets out a clear framework to support the strategic implementation of evidenced based suicide prevention initiatives.”
– Executive Director Gold Coast Mental Health and Specialist Services, Malcolm McCann
The Queensland Alcohol and Other Drug (AOD) Network has completed a state-wide mapping process of all AOD services and funding to define improvements in commissioning, service quality and service outcomes. Key recommendations achieved in the review in 2021/22 are:
read more
The Alcohol and Other Drugs (AOD) GP support project aims to support the delivery of drug and alcohol training packages to the primary health care sector, including supporting GPs and other health professionals to enhance their knowledge and application of the AOD referral pathway and increase awareness of evidence-based resources to improve drug and alcohol addiction treatment.
|
|
read less

The Strengthening Health Assessments Pathways for Children and Young People in Care is a Queensland-wide project aimed at improving both the child safety and health sector response to the health care needs of young people in care.
Funded by the Department of Children, Youth Justice and Multicultural Affairs until 2023, Primary Health Networks across the state and child safety services centres are leading this key system reform at a local level.
This includes ensuring that GPs are applying the National Clinical Assessment Framework for Out of Home Care, improving access and timeliness of health assessments and improving integration and information sharing between health practitioners, the Department of Child Safety, families and carers.
read more
Stakeholders
|
|
read less

Primary Sense is a population health, data extraction, analysis, reporting and decision assist tool for general practice that has been pioneered by Gold Coast Primary Health Network (GCPHN). Its’ wide-reaching success locally has seen it being rolled out at a national level. GCPHN is supporting the WA Primary Health Alliance (WAPHA) to implement this national rollout with 17 Primary Health Networks providing funding for a national scaled version of Primary Sense. Ten PHNs nationally (including Gold Coast) are planning to transition to the national, scale version of Primary Sense by June 2023.
This toolset assists general practices to identify patients most at risk of poor health or disease and provide targeted interventions to reduce their risk of becoming unwell or experiencing a preventable hospitalisation.
read more
“It’s great to know the Primary Sense prompts I receive are specific to each patient and so easy to action.”
– General Practitioner
|
|
read less
“Primary Sense was mentioned by Michael Brennan, Chair of the Productivity Commission, at the CanForum at Parliament House in Canberra, as a great example of innovation, with doctors on the Gold Coast working together to solve a problem through innovation and data.”
In partnership with Queensland Health, we fund the Way Back Support Service, run by Wesley Mission Queensland, which provides three months of tailored non-clinical psycho-social support to people who have recently attempted suicide or are at risk of suicide, who have been admitted to Gold Coast Health hospitals.
Support facilitators guides participants through their recovery including helping build a personalised safety plan and linking them to health and community services and clinical care if needed.
read more
“I was in care of (Support Facilitator) of Wesley Mission Queensland for several months. It was incredibly positive experience. (Support Facilitator’s) high professionalism, kindness, will to help his client, literally saved my life and helped me to get back on my feet. (Support Facilitator) was not afraid to go the extra mile to help me, in fact, they went one hundred extra miles to help me with my very difficult and complicated life situation, to get me out of the darkness of my completely destroyed mental state. They was the first to believe in me. Piece by piece, they helped me to build my life back together, to feel that I am a human being again. Their kind words and their determination to help left me no other option than to get on the path to recovery. What a journey it was! Thanks that there are organisations like Wesley Mission and people like [Support Facilitator] on this planet. Thank you from the bottom of my heart.”
– Client feedback
To support people in the Gold Coast community who may experience mental health concerns outside regular business hours and as an alternative to emergency department presentations, we have established After Hours Safe Space services which operate after hours. The first service was opened at Mermaid Beach in 2018.
In response to high demand and with Queensland Health funding, we worked with Gold Coast Health (GCH) for another low to moderate intensity community-based service. Through co-design with GCH, we further developed our regional model and launched a new service in Southport in late 2021. The Mermaid Beach service remains operational with some changes to align with the Southport site. Both sites are operational seven days a week. Consumers can walk into a warm and welcoming café style environment with access to face-to-face supports form lived experience workers. Additional support is available from a specialised mental health clinician if required.
read more
Achievements
|
|

read less
For the last eight years we have commissioned PainWise to run the Turning Pain into Gain program which has been heralded as life changing by participants.
The program provides pain management services to patients through a multi-disciplinary team including a GP, pharmacist, dietician, pain educators, counsellor and psychologist. It also provides individual and group sessions either face-to-face or through telehealth services.
The program also delivers training to healthcare professionals to ensure their knowledge and skills on pain management are up-to-date.
read more
Achievements
Service Provider
Stakeholders
|
|
read less
 “The Turning Pain into Gain pain program is an incredible program, which is in my eyes, unique. It looks at each person as an individual maintaining a holistic approach. For me personally it’s not just about the consultations that I receive, it’s the ongoing care afterwards including referrals and the management plan which exceeded my expectations. The group activities are amazing and allows you the opportunity to meet people if you wish and share your stories and receive what I call ‘take aways’. As a result of being part of the TPIG program, I have become a committee member of the local FM/ME/CF support group to give back to others what I have learnt. Most importantly my voice has been heard.”
“The Turning Pain into Gain pain program is an incredible program, which is in my eyes, unique. It looks at each person as an individual maintaining a holistic approach. For me personally it’s not just about the consultations that I receive, it’s the ongoing care afterwards including referrals and the management plan which exceeded my expectations. The group activities are amazing and allows you the opportunity to meet people if you wish and share your stories and receive what I call ‘take aways’. As a result of being part of the TPIG program, I have become a committee member of the local FM/ME/CF support group to give back to others what I have learnt. Most importantly my voice has been heard.”
– Kerrie Thomson, 2022 Participant
The Integrated Team Care Program has been improving healthcare coordination for Aboriginal and Torres Strait Islander community members in the Gold Coast region for many years. The program has two service areas, one which provides support and service for people with long-term chronic health conditions (complex care pathways) and the second program focussing on support.
The program is commissioned through Kalwun Development Corporation and includes Indigenous project officers, outreach workers and care coordinators, who aim to close the gap in life expectancy by improved access to culturally safe mainstream primary, community and tertiary healthcare services for Aboriginal Torres Strait Islander people.
read more
Healthcare support
Transport services
Cultural awareness training
|
|
read less
“Assisted an elderly lady who presented to the Krurungal office before opening hours. The Service Coordinator identified the person was unwell and disorientated and travelled with local police and the client to the hospital to ensure her health and safety and connection to services.”
We were one of three Primary Health Networks nationally to receive funding for a wound management pilot. This program supports people living in Residential Aged Care Facilities (RACFs) with chronic wounds, with the intent to build the capacity of RACF staff to deliver evidence-based wound care onsite.
The project is led by an experienced Wound Management Nurse Practitioner and includes:
read more
 Achievements
Achievements
|
|
read less
“A patient had a non-progressing stage 3 pressure injury on the heel. Wound healing is now anticipated within the next four weeks, attributable to the implementation of advanced wound dressing products, appropriate pressure injury prevention and management strategies and appropriate wound interventions. The RACF clinical staff involved have reported improved confidence in managing similar wounds in the future.”
 We fund a dedicated primary care based wound clinic led by a wound specialist GP and nurse practitioner, who are supported by a team of highly trained nurses. The Chronic and Complex Wound Clinic supports local GPs and their patients to improve health outcomes with people that have chronic, complex, recurrent and debilitating wounds that seriously impact their quality of life.
We fund a dedicated primary care based wound clinic led by a wound specialist GP and nurse practitioner, who are supported by a team of highly trained nurses. The Chronic and Complex Wound Clinic supports local GPs and their patients to improve health outcomes with people that have chronic, complex, recurrent and debilitating wounds that seriously impact their quality of life.
read more
|
|
read less
“A visitor to the Gold Coast presented to the Bundall Medical Centre wound clinic (referred by a local GP she had seen) with a wound of more than four months duration. The correct diagnosis was made quickly (arterial insufficiency), whilst working with their GP and Gold Coast Health, an urgent stent was completed. This saved the person’s limb and the wound healed in five weeks.”
The Wound Education and Training Program offers training and education that will increase confidence, knowledge and skills of GPs and nurses responsible for the care and management of patients living with chronic and/or complex wounds in general practice or residential aged care settings.
read more

|
|
read less
The Gold Coast Referral and Triage Service has been a central point for receiving and assessing referrals for people requiring mental health and suicide prevention services that are not in crisis. In the last 12 months the service has:
From July 1, 2022, this service has transitioned to the Gold Coast National Head to Health Intake and Assessment Phone Service.

The Expanded Horizons Program is a peer led program that works to ensure young people in the Gold Coast region that identify with the LGBTIQAP+ community have a place of connection and access to psychosocial programs and supports. The program offers resources, guest speakers, peer support and information to build a positive sense of identity and connection.
read more
read less
The Community Pathway Connector program simplifies and improves the process to connect services for members of the Gold Coast community requiring culturally appropriate mental health and well-being services. CURA has been providing services for people from culturally and linguistically diverse backgrounds and Krurungal, for Aboriginal and Torres Strait Islander peoples. The service connects people of any age with mental health and wellbeing services, removing any barriers to ensure they receive culturally safe access to support services.
read more
Service Provider
read less
“Krurungal client successfully supported with multiple services, to navigate the complexity of the health and services system. Client was able to live safely, connected to services to support her and employment. Client was assisted with documentation support, advocacy with QPS and cultural liaison unit – in language. Client was met with dignity, respect and offered flexible service delivery, available with the model of the CPC program.”
We have progressed work on the Psychological Services Program review to establish a new service model in late 2022, with a focus on identifying areas for improvement in the following key areas:
headspace provides a range of services to improve the health and wellbeing of young people aged 12-25. This includes mental health and wellbeing, physical and sexual health, work and study support and alcohol and other drug services.
We commission Lives Lived Well to run headspace Southport and headspace Upper Coomera, which opened in July 2020.
read more

read less
“A 17 year old reported experiencing anxiety at school and was struggling with feelings of depression and having difficulty setting realistic career goals. The clinician provided two targeted brief intervention sessions providing psycho–education related to coping strategies to combat negative thinking and a discussion of career goals. This facilitated the young person to make some decisions about their career pathway and set realistic goals. Anxiety issues resolved and the young person was feeling more positive about their future.”

With approximately 39% of all permanent aged care residents living with mild to moderate depression, and as a national priority, we commission Change Futures to provide psychological support to residents in residential aged care facilities (RACFs).
The service supports residents experiencing mild depression of anxiety and those having trouble adjusting to changes or coping with loss. The service can also support people experiencing dual diagnosis of mental health and dementia or brain injury/development disability, where behaviours are identified as mental health related.
Sessions can be focused on transitions into aged care, engagement and wellbeing and managing identified mental health conditions.
COVID-19 has presented considerable challenges for residents with additional lockdown measures, increasing feelings of isolation and anxiety and in these instances, support has continued through telehealth options.
“We very much appreciate Change Futures coming to us. Our residents benefit from your services greatly. The practitioner that visits our facility is very professional and assists our resident with depression and anxiety especially during COVID times. Our residents often express positive thoughts after sessions with your practitioners. Not only does this benefit the care staff, but also benefits the residents, their families, and the community. Thank you.” – RACF Clinical Manager
read more
read less
Developed by Beyond Blue, NewAccess is a low intensity mental health coaching program, designed to provide accessible, quality services for anyone finding it hard to manage life stress. People can access six coaching sessions either face-to-face, telephone or video link. Coaches assess the person’s needs, then work with them in setting practical, effective strategies to help them get back on track.
“Prior to the program I questioned whether my feelings were valid but since talking to you I know they are legitimate and valid which feels good to acknowledge that. If those feelings do come back, I will now be more aware of what is happening, and I will be a step-in front of them after the program as I now have new tools and strategies to help.” – Client
read more
read less
headspace Early Psychosis supports young people aged 12-25 at risk of, or experiencing, their first episode of psychosis. In addition, the Lighthouse multi-disciplinary team works with young people aged 12-18, providing longer term support to help them better manage the impacts and symptoms of past complex trauma and work towards creating positive life changes.
read more
headspace Achievements
Lighthouse Achievements
read less
Examples of achievements by young people who joined the program with significant low functioning including poor school attendance and limited capacity to gain employment.
read more
Home based care through Mobile Assessment Treatment Team, (MATT) transitioned to Continuing Care Team (CCT) and was supported into a hospital admission with interagency working with public health systems.
The teenage client with symptoms indicative of an episode of psychosis was referred by a private psychiatrist seeking case management. Assessment with a psychiatric registrar and culturally appropriate. MATT clinician was arranged within 48 hours, with advice given to the family around crisis options. It was determined that Home Based Care appointments were the least restrictive option for managing the episode, including twice weekly psychiatric reviews for a period of two weeks with a further period of joint MATT/CCT intervention to support transition from Home Based Care to case-management. The joint approach allows a greater frequency of contact with the young person and family and promotes engagement and trust in the service.
The Home-Based Care interventions included:
With a decline in the client’s mental state, they were assessed by the psychiatrist at hEP and placed under the Mental Health Act for assessment and admitted to an inpatient ward. Due to the education and support the family had received they were supportive of this intervention and well placed to provide additional support.
At the time of writing, the client’s case manager from hEP CCT is liaising with the inpatient treating team to ensure the discharge plan for this young person meets their needs, and that any transfer back to hEP is seamless.
read less
The Clinical Care Coordination program provides holistic, high-intensity support services for those living with the impacts of complex and mental illness. Through comprehensive care co-ordination, clients are supported towards recovery.
A multidisciplinary care team (of mental health professionals) support clients to achieve their identified goals holistically by including and addressing social determinants of health and key life stressors such as housing, financial issues, unemployment, health issues, lack of appropriate mental health clinical supports, access to benefits, transport and legal issues, and feeling connected to others in community. This promotes stabilisation of mental health and empowers self-efficacy and quality of life.
read more
Clients require a GP or private psychiatrist referral to access the service and are then offered brief to moderate length supports which includes a holistic needs assessment, customised care planning, and referrals to appropriate locally based (public and private) health and social services and enrolment into social activities etc. Most clients receive support for 3-9 months, ensuring a stepped care approach that recognises the variability of an individual’s mental ill-health presentation at any one time, and that a continuum of service interventions is necessary to offer the right service at the right time.
While in the program, clients may seek assistance to apply for NDIS supports. When support has completed, clients can be on-referred for ongoing supports as required to moderate or low intensity services.
read less
“My quality of life has improved. My home environment has changed for the better, as well as being more social, without you guys I wouldn’t be socialising at all. Before Plus Social, I used to sit at home with doors, curtains closed in the dark all day. Now I don’t get as much anxiety when I go to the front door, I let air and light into the home.”
– Client feedback

The Psychosocial Services program is a non-clinical service providing low to moderate intensity individual and group activities to support people to achieve their mental health recovery goals.
The service offers a range of group activities that aim to build capacity and stability in areas such as:
read more
read less
“I am now more willing to reach out for help. I don’t feel so scared to attend groups as I realise the people attending are just like me. I used to think I’d get judged for having a mental illness but now I realise everyone attending has their own story and are just every-day people.”
With a number of alcohol and other drug (AOD) services on the Gold Coast at capacity and the difficulty for many people to access residential services due to family or work commitments, this pilot program provides more accessible options for people with symptoms of AOD withdrawal.
Individuals are supported to withdraw from a range of substances in their own homes with the support of specialist AOD clinical staff, family and support person, or at the service.
read more
read less
“Handing my life over for a week to a caring team of professionals that know what is best for me. This support is ongoing with counselling, workshops and access to other services. I’m truly grateful for this program and the team that run it.”
– Program participant
read more
This program provides community-based alcohol treatment services on the Gold Coast for adults aged 18 years and over. This service is for individuals that are experiencing substance related disorders who find it easier to access services out of usual business hours.
Kalwun Social Health Clinical Care (Alcohol and Other Drugs)
This low to high intensity service offers comprehensive support for Aboriginal and Torres Stair Islander people who are experience some mental health challenges or for those alcohol and other drug needs. The program works within a social and emotional wellbeing framework and provides clinical and non-clinical treatment.
The services empowers people to self-manage and make decisions about their own health at their own pace. The Social Health Team offers a person and family approach to providing care and can link clients to a range of internal and additional services.
Achievements
Service Provider
This program provides Gold Coast youth and adults, a range of service options to support their needs through community-based alcohol treatment services. Support is also available for their families/carers. Service streams offered are family therapy and support, youth outreach, transition support (from AOD residential treatment to community living) and youth dual diagnosis. Treatment options are provided through outreach, co-location arrangements and a centre-based service delivery at Burleigh Heads and Nerang.
read less
We provide support to general practices, the cornerstone of primary care, in their provision of high-quality care for Gold Coast residents. The support provided ranges from working with general practice teams implementing data informed quality improvement (QI) activities to providing access to information and resources through a dedicated phone and email support line, newsletters and the Gold Coast Primary Health Network (GCPHN) website.
We play a key role in raising awareness in the Gold Coast community about the importance of participation in the national bowel, breast and cervical cancer screening programs, and supporting quality improvement initiatives for general practices, to promote screening among their patients.
read more
read less
Results for participation rate for the eligible population in the national cancer screening programs for the region and nationally.
Gold Coast |
National |
|
| Bowel Cancer Screening (eligible population 20-69 years) |
37.6% | 41.6% |
| Breast Cancer Screening (eligible population 50-74 years) |
49.9% | 49.9% |
| Cervical Cancer Screening (eligible population 50-74 years) |
55.9% | 55.7% |
Source: AIHW, National cancer screening programs participation data Bowel and breast cancer: 2019/2020 Cervical cancer: 2018/2020
We have continued to support general practices to keep immunisation levels high, to better protect local residents against disease and have played a key role in influenza immunisation and the COVID-19 vaccination program.
read more

ACHIEVEMENTS
read less
We have been part of the Queensland Government funded My health for life program since 2017. This program helps Queenslanders at risk of developing chronic conditions, including type 2 diabetes, heart disease and stroke, to live well and reduce their risk factors by making lifestyle changes such as healthy eating and increased physical activity.
read more
|
|
Since 2005, we have been instrumental in helping shape the future of the primary health workforce. Partnering with Griffith, Bond and Southern Cross universities, we help train the next generation of GPs and practice nurses, by placing medical and nursing students in general practices across the Gold Coast, northern NSW and Brisbane.
Medical Placements
Nurse Placements
Specialist Placements
|
|
read less
“Everyone at the clinic was approachable, knowledgeable, and willing to teach. The community in which the practice serves is very appreciative of the clinic’s work, and this was reflected in the care provided not only by the clinicians but also receptionists and the clinic management team. The clinic is central to a very underserved diverse patient population and this itself has provided lots of learning opportunities. I am appreciative for having had the opportunity to learn from Dr X, Dr Z, Dr Y, Dr S, Dr N and Dr D. Not only did they provide plenty of opportunities for clinical learning through patient interactions, they took the time to teach and discuss certain topics that I wasn’t very confident with in their own time. Most of all they shared their own experiences through medicine and general practice, which helped provide some perspective for my own career path. They are all very passionate about making a difference to the community in which the clinic serves and am constantly trying new ideas to improve care delivery. The nurses were also very approachable and happy to teach. This placement has certainly cemented my decision to pursue general practice in future because of the experiences I have gained from this placement.”
– Bond Student

Gold Coast Primary Health Network (GCPHN) has implemented a number of initiatives to engage with general practice staff and healthcare providers to promote quality improvement initiatives and digital technologies. This has included promotion and education about digital health tools such as Smart Referrals, HealthPathways, My Health Record (MHR), telehealth, electronic prescribing and secure messaging.
read more
Achievements
Stakeholders
|
|
The Gold Coast PHN hosted an event for specialist practices on 12 July 2022. The event attracted a range of specialists and practice managers and gave attendees an opportunity to hear from our own local specialists about the benefits and how they have been using My Health Record.
read less

In response to the Royal Commission into Aged Care Quality and Safety, the Commonwealth Department of Health has developed and funded a more significant program of work that will see Primary Health Networks managing a number of new aged care activities.
We have been allocated new funding of over the next four years (from 2021/22), to use our existing expertise and relationships with local health service providers to commission a range of activities to keep people at home, delaying entry into aged care facilities and reducing avoidable hospitalisations for senior Australians.
The focus for this year has been in working collaboratively with our stakeholders in the planning, which has included undertaking needs assessments, service mapping and scoping of evidence-based models for implementation in the next financial year. A brief outline of the aims of each of the programs is outlined below.
read more
 We will be assisting participating residential aged care facilities to have access to telehealth facilities, equipment and training for staff to enable their residents to have video consultations, when needed, with their primary health care professionals, specialists and other clinicians.
We will be assisting participating residential aged care facilities to have access to telehealth facilities, equipment and training for staff to enable their residents to have video consultations, when needed, with their primary health care professionals, specialists and other clinicians.
This project aims to support participating residential aged care facilities to implement individualised after-hours management plans, in line with residents’ wishes and to be aware of after-hours health care options and referral pathways and utilise these when needed.
In May 2021, Gold Coast Health implemented an electronic platform, Gold Coast Community HealthPathways, where GPs can access clinical and service referral pathways for specific medical conditions or health needs. This project is a partnership between Gold Coast Health and Gold Coast Primary Health Network to develop and launch a wide range of specific aged care and dementia pathways.
The aim of this initiative is to support people living with dementia to live well in the community for as long as possible, through easy access to information on dementia diagnosis and initial and ongoing services and supports to people living with dementia, their carers and families. This will help to support them to plan ahead to better navigate their dementia journey.

We are supporting the development of a new workforce called ‘care finders’ who will provide specialist and intensive assistance to help people to understand and access aged care services and connect with other relevant supports in the community. Navigating the aged care system is complex, and the target group for this program will be those who require more intensive support and include some of our most vulnerable people in the community. The care finders will ensure these people have access to the most appropriate aged care supports and services by working with them and building rapport and trust. Once services are commenced, the care finders will provide follow up to ensure needs are being met. The service will commence in January 2023.
Senior Australians are being supported to live in the community for as long as possible and minimise some avoidable risks of early entry into residential aged care. As part of the planning, we will explore services or supports to prevent, identify, and reduce chronic disease and health issues, avoid inappropriate hospital admissions and improve health outcomes for senior Australians.
read less
During 2021-2022, we supported activities for palliative care patients at home or living in residential aged care facilities (RACFs) and their staff, to improve their quality of care and their end-of-life experience.
|
|
read more
 Funded by the Commonwealth and state government with additional funding from Gold Coast Primary Health Network (GCPHN), the Gold Coast SPACE project provides RACFs with education, training and capacity building through the innovative use of ‘Palliative Care Needs Rounds’, which are triage meetings with RACF staff and clinicians, focusing on residents at risk of dying without as plan in place.
Funded by the Commonwealth and state government with additional funding from Gold Coast Primary Health Network (GCPHN), the Gold Coast SPACE project provides RACFs with education, training and capacity building through the innovative use of ‘Palliative Care Needs Rounds’, which are triage meetings with RACF staff and clinicians, focusing on residents at risk of dying without as plan in place.
Funding to extend this program has enabled additional staff allocation and expanded service delivery to more RACFs and residents.

 We received pilot funding to improve the coordination and integration of end-of-life care across primary, secondary, tertiary and community health services to support patients who wish to receive palliative care in their home environment. The program has now been funded until June 2025, with the focus on building the workforce capability of primary care workers in palliative care and bereavement support.
We received pilot funding to improve the coordination and integration of end-of-life care across primary, secondary, tertiary and community health services to support patients who wish to receive palliative care in their home environment. The program has now been funded until June 2025, with the focus on building the workforce capability of primary care workers in palliative care and bereavement support.
read less
 The Gold Coast Primary Health (GCPHN) website, www.gcphn.org.au plays an important role in providing timely, accurate and evidence based information and resources to health professionals and the local community. The website has continued to build a strong domain reputation as a trusted source of information.
The Gold Coast Primary Health (GCPHN) website, www.gcphn.org.au plays an important role in providing timely, accurate and evidence based information and resources to health professionals and the local community. The website has continued to build a strong domain reputation as a trusted source of information.
User numbers have been very high throughout the pandemic as general public and health professionals sought reliable information in frequently changing circumstances. Some of the information that has been curated for local health professionals includes COVID-19 management pathways, downloadable patient resources, latest updates and alerts and vaccination information. The COVID-19 pages were also one of the most viewed by community members with information about testing, vaccination and living with COVID.
read more
|
|
read less
“GCPHN is a trusted source of information for the Gold Coast primary health care sector.”
– Website feedback
 We play an integral role in the development of the primary healthcare workforce with training, education and communication to ensure health professionals have access to the latest information to provide the highest level of patient care.
We play an integral role in the development of the primary healthcare workforce with training, education and communication to ensure health professionals have access to the latest information to provide the highest level of patient care.
Our training activities are aligned with quality improvement activities and are accredited.
We have commissioned Australian General Practice Accreditation Limited (AGPAL) to develop an online eLearning platform to build internal and external workforce capability to achieve high performing primary care on the Gold Coast, through upskilling general practice and GCPHN staff in core quality improvement training. In the last 12 months:
read more
 We often partner with industry leaders, to support online and face-to-face education and training events across a range of topics and areas with an emphasis on priority health needs and quality practice. In the last 12 months some topics have included:
We often partner with industry leaders, to support online and face-to-face education and training events across a range of topics and areas with an emphasis on priority health needs and quality practice. In the last 12 months some topics have included:
|
|
Stakeholders
|
|
read less
“The presentation was very powerful and convinced me that we need to get in board with this – I was on the fence previously.”
(My Health Record) – Specialist participant feedback
GCPHN Financial Statements for the year ending 30 June 2022
So we can provide you with the most accurate information,
please tell us a little more about yourself

