



To receive important alerts and updates from Gold Coast Primary Health Network, please submit the form below.
"*" indicates required fields

To receive important alerts and updates from Gold Coast Primary Health Network, please submit the form below.
Dr Magazine is circulated to GPs and specialists throughout South East Queensland, including Gold Coast, Sunshine Coast, Brisbane and Moreton Bay.
To get in touch, please email Murray McGregor.
As a general practitioner or clinician, you’re at the frontline of patient care, and ensuring people receive the right mental healthcare at the right time is crucial to their treatment and recovery journey.
The Initial Assessment and Referral – Decision Support Tool (IAR-DST) offers a standardised, evidence-based approach to mental health referrals, helping you confidently recommend an appropriate level of care that matches a person’s mental health needs.
Guided by your own assessment and clinical judgement, the IAR-DST provides a consistent decision-making framework for appropriate referrals.
Through the IAR-DST training offered by Gold Coast Primary Health Network (GCPHN), you can learn how to make the most of the IAR-DST and enhance your day-to-day clinical practice.
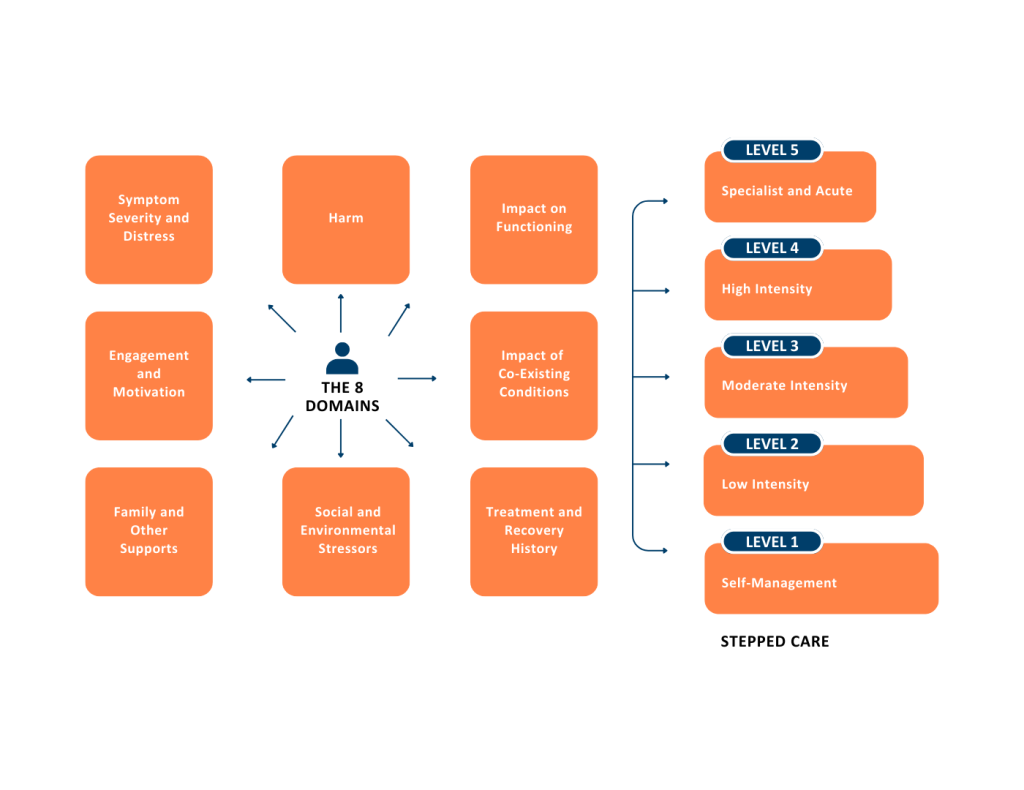
Whether a person has mild or severe mental health needs, the tool helps you gather essential information through the application of eight holistic assessment domains, that are used to match a person to one of five appropriate levels of care with varying degrees of intensity.
GCPHN commissions a range of local Gold Coast mental health services across these five levels of care, from low intensity services for mild conditions to high intensity interventions for those with severe or persistent mental health issues.
As a GP or health professional, the IAR-DST is a beneficial tool to reduce any risks associated with underservicing or overservicing a person and can support you to expand upon your existing referral pathways with confidence.
Dr Jardin Taha, a working GP at Burleigh Heads, recently completed the IAR-DST training.
“This tool helps clinicians assess mental health needs and decide the best level of care for the patient using an evidence-based framework,” he said.
Completing the two-hour online IAR-DST training workshop equips you with key skills including:
GPs and GP Registrars who complete the training will earn RACGP CPD hours (1.5 hours in Educational Activities and 0.5 hours in Reviewing Performance) and receive a $300 reimbursement* for their time.
Mental health needs can be complex and challenging to navigate, but the IAR-DST is designed to recommend the appropriate intensity of care for your patient. By utilising this tool, you’ll be able to confidently guide patients toward the care they need.
Don’t miss this opportunity to enhance your expertise, earn CPD hours and improve mental health outcomes for your patients.
| Scan the QR code or visit www.gcphn.org.au/patient-care/mental-health/iar-dst to register for one of the upcoming workshops or request a session at a time that suits your practice. |
 |
This article was distributed in the September/October 2024 edition of Doctor Magazine.
Gold Coast Primary Health Network Chair Dr Lisa Beecham says the Gold Coast community is missing the point with immunisation at the same time influenza circulating in the city is at its most infectious.
According to the latest figures by Primary Health Network, the Gold Coast has some of the lowest child immunisation rates in the country against highly infectious diseases such as measles, chickenpox, whooping cough and more.
“Vaccine complacency is having a serious impact on our local hospital emergency departments, where we are seeing large numbers of presentations with COVID-19, influenza, asthma, emphysema, and child admissions,” Dr Beecham said.
“It’s at a rate that’s putting the health of some of the youngest and most vulnerable people in the community at risk, so it’s more vital than ever that healthcare professionals address vaccine complacency and improve vaccine literacy among parents,” she said.
Dr Beecham said healthcare providers can use several available resources to improve immunisation rates.
“The SKAI website offers excellent tools for facilitating conversations with patients and addressing their concerns,” Dr Beecham said.
“Additionally, the Primary Sense Child Immunisations report can help GPs and nurses identify infants and children who are due or overdue for immunisations, enabling more targeted discussions with parents.
“By actively promoting immunisation, educating patients, and utilising available resources, healthcare professionals can make a significant impact on public health.
“It’s all about us ensuring immunisation rates rise to protect not only our individual patients but also the broader community, reducing the burden on the healthcare system and safeguarding the health of the most vulnerable,” she said.
Visit www.gcphn.org.au/patient-care/prevention/immunisation for additional immunisation information.
Latest figures source: www.health.gov.au/resources/publications/2023-phn-childhood-immunisation-coverage-data
This article was distributed in the July/August 2024 edition of Doctor Magazine.

Tony McCormack, a former crane operator from Currumbin, knows firsthand the lifesaving power of bowel cancer screening.
When a free bowel screening kit arrived in the mail on his 58th birthday, his wife Tanya said, “Right, Happy Birthday. You’re doing it.”
This simple yet decisive action set off a chain of events that would ultimately save Tony’s life.
“After the test detected blood in my faeces, I went to my GP who referred me to a colorectal surgeon who performed a colonoscopy at Tugun’s John Flynn Hospital,” Tony said.
“It revealed bowel cancer at the base of the colon.”
Despite the challenges of nine months of intensive chemotherapy and radiation, Tony remained resilient, supported by his family, friends and medical team.
“The early detection gave the doctors the chance to stop it in its tracks without surgery,” he said.
Today, Tony is clinically clear and grateful that a routine screening test saved his life.
According to the Cancer Council, bowel cancer is one of the most common cancers in Australia and the second highest cause of cancer death. Each year around 400 Gold Coast residents are diagnosed with the disease.
Despite its prevalence, national screening participation rates remain low at about 40 per cent. If found early, almost all bowel cancers can be successfully treated.
Tony’s story highlights the pivotal role healthcare professionals play in encouraging participation in bowel screening programs. By educating patients about the importance of early detection and facilitating access to screening tests, healthcare professionals can help combat this prevalent yet treatable disease.
Initiatives like the Australian Government National Bowel Screening Program aim to increase and encourage early detection, with eligible Australians aged 50 to 74 mailed a free test done at home every two years.
Visit www.health.gov.au/nbcsp to learn more about the program and how to access kits to issue to eligible patients.
This article was distributed in the May/June 2024 edition of Doctor Magazine.
Childhood immunisation rates across the Gold Coast region have declined over the last three years, falling below the critical 95% target required for herd immunity.
During the last quarter of 2023, 87 percent of Gold Coast children were fully immunised at one year of age, compared to 92 percent in the last quarter of 2019.
Gold Coast Public Health Unit Medical Director Dr Kate Alexander said this same declining trend is seen for children at two and five years of age.
While coverage rates for Gold Coast First Nations children in the same period were higher than all children, the rates are also declining. The same trend is seen across Queensland, Australia and internationally.
Dr Alexander warns that the resurgence of diseases like pertussis and measles in the South East, coupled with decreasing immunisation coverage, leaves the community vulnerable to outbreaks of preventable diseases.
“Several well-known behavioural and social factors contribute to this decline, ranging from perceptions of disease risk and vaccine confidence to social norms, community support, and healthcare accessibility,” said Dr Alexander
She said the ongoing COVID-19 pandemic has added new challenges, with families reporting difficulties in accessing GP appointments and expressing reluctance to bring healthy children into medical settings due to fears of COVID-19 exposure.
“Other issues including vaccine availability, affordability, accessibility, and the overall healthcare experience also influence the uptake of recommended vaccines.
Research, such as the UNICEF Vaccine Confidence Project, highlights the broader impact of the pandemic on childhood immunisation, showing a 7.5% drop in Australia’s confidence in childhood vaccinations from pre-pandemic levels.
“Studies indicate that primary healthcare recommendations, particularly those from GPs and primary care nurses, play a pivotal role in influencing parents to immunise their children.
“Primary care reminders motivate families to adhere to the National Immunisation Program schedule, ensuring timely protection against serious diseases,” said Dr Alexander.
| In response to the decline in childhood immunisation rates, the Gold Coast Primary Health Network and Gold Coast Public Health Unit have been working collaboratively additional immunisation activities in the Gold Coast region. |
These include pop-up immunisation clinics at Burleigh State School markets on Saturdays during December and January.
“We are also supporting five primary practices in the Broadbeach-Burleigh and Coolangatta areas to run Australian Immunisation Register 10A provider reports to identify and follow up children in their practice who are overdue for immunisation, as well as undertaking a World Health Organisation Tailoring Immunisation Programmes (TIP) project in postcode 4209 on the northern Gold Coast to explore barriers and enablers to immunisation among parents, vaccine providers and community leaders,” said Dr Alexander.
| The Gold Coast Primary Health Network has initiated public health promotion activities about the benefits of childhood immunisations as well as sponsoring specialist immunisation training for practice nurses. |
As childhood immunisation rates continue to plummet and vaccine-preventable diseases resurface, a collaborative effort between primary care, child health services, and public health becomes imperative.
The focus must be on supporting families to ensure their children are immunised on time, reinforcing the crucial role that primary care plays in securing community health.
| Gold Coast General Practices requiring further information can contact the Practice Support Team at the Gold Coast Primary Health Network on email practicesupport@gcphn.com.au or phone 07 5612 5408. |
This article was distributed in the March/April 2024 edition of Doctor Magazine.
Gold Coast Primary Health Network (GCPHN) is shaking up the narrative around ageing with the launch of three innovative healthy ageing programs, available at no cost to eligible Gold Coast residents.
These programs challenge the notion that frailty is an inevitable part of ageing and are designed to empower individuals to enhance their overall quality of life and live longer independently.
Frailty is often dismissed as an unavoidable part of growing older.
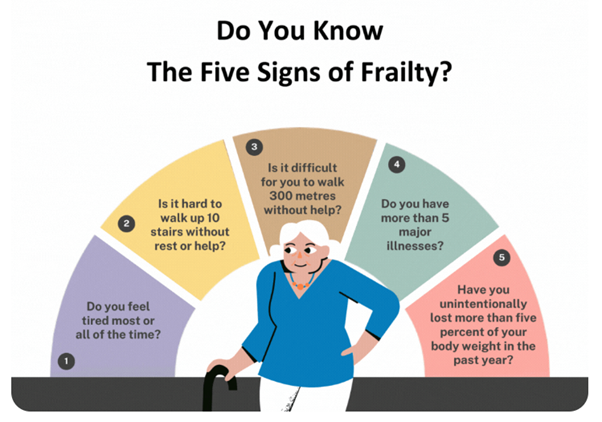
Recognising the five common signs of frailty – fatigue, weakness, mobility challenges, major illnesses, and unintentional weight loss – highlights the silent indicators preceding a decline in an individual’s health.
With even one sign of frailty, individuals risk losing their ability to bounce back from an illness or accident.
Gold Coasters can now access three distinct programs designed to equip them with the knowledge and tools to combat the signs of frailty, improve their quality of life and maintain independence.
BUnyAH Interprofessional Healthy Lifestyle Program
A collaborative effort between Bond University Allied Health Department and Avanti Health Centre, this program combines health education and exercise classes. Participants engage in two sessions a week for 12 weeks, complemented by a gym membership for the program’s duration. The holistic approach includes group education sessions, exercises, and individual therapies.
Frailty Care in the Community Program
Developed and executed by allied health professionals, this program focuses on managing and preventing frailty through awareness and therapies. The program aims to reduce the risk of falling and losing independence through individual appointments and group-based movement sessions.
Each participant is assessed for their nutrition, medication, cognition and mental health and a program is tailored according to their needs.
The Frailty in the Community Program is conducted either at the participant’s home or in a small group environment. The program consists of six sessions across four to six months plus there is a further six months of support available afterwards.
Mungulli Yarn and Walk Program
Led by Gold Coast Health, this culturally specific outdoor physical activity and education program is tailored for First Nations people. Limited to 10 participants per program, it explores cultural activities, healthy eating, health conditions and risk factors, with light physical activity, including walks.
These programs are not merely about managing frailty; they symbolise a transformative power, enabling older individuals to lead healthy lives in the comfort of their homes.
Early intervention in ageing is a vital component in addressing health issues, preventing chronic conditions, and preserving independence.
To join a healthy ageing program, Gold Coast residents can participant by obtaining a referral from a GP or allied health professional.
| More information is available at gcphn.org.au/iamnotfrail |  |

This article was distributed in the January/February 2024 edition of Doctor Magazine.
With Australia on track to be the first country to eliminate cervical cancer by 2035, there is a concerted effort to educate people about the importance of vaccination and screening against cervical cancer.
Deaths from cervical cancer and the number of new diagnoses have halved since the National Cervical Cancer Screening was first implemented in 1991.
However, in Queensland, around 200 people are diagnosed with preventable cervical cancer each year.
Australia-wide, around 70 per cent of patients diagnosed with cervical cancer were not up to date with screening.
Cervical cancer prevention has never been more accessible with just one dose of the human papillomavirus (HPV) vaccine plus cervical screening every five years being lifesaving initiatives.
The cervical screening procedure, which replaced the invasive Pap test in 2017, tests for the HPV infection, which is the cause of almost all cervical cancers.
A HPV vaccine is offered to all students through the school immunisation program in early high school. A free catch-up program is available for people aged 25 years or younger.
After vaccination, five-yearly screening from the age of 25 is the best chance of detecting this cancer early and implementing effective treatment.
The self-collection option of cervical screening is a game changer for women and people with a cervix who find the standard cervical screening process difficult or confronting as they can now take their own sample from their vagina using a simple swab in a private space at their local general practice.
Primary Sense a population health management and clinical audit tool , which is provided by GCPHN to GC practices for free can be used to identify patients who are due or overdue for screening. Patients can then be invited in for a cervical screening appointment and offered the different options for screening.
MBS statistics over the past year indicate the number of women accessing self-collection is doubling each quarter.
The data shows that people aged between 30 and 74 who had never had a cervical screening test before were getting tested with one-in-five of these choosing to self-collect their sample.
In older cohorts, the preference for self-collection for women aged between 60 and 69, who had never screened before, was one-in-three.
Because cervical cancer can take up to 10-15 years to develop, the early detection of HPV and cell changes means it may be possible to prevent HPV infection developing into cervical cancer.
One dose of the HPV vaccine and cervical screening every five years can protect people from cervical cancer.
The HPV vaccine is available free of charge to all young people aged 25 years or under.
This one vaccination plus screening tests every five years for people aged between 25 and 74 is all it takes to maximise protection.
The National Cancer Screening Register (NCSR) is a single electronic record for each Australian taking part in the bowel and cervical screening programs.
Practices can integrate their clinical software (Best Practice Premier or Medical Director Clinical) with the NCSR, which brings the following benefits:
This article was distributed in the November/December 2023 edition of Doctor Magazine.
We’ve heard the statistics and it never gets easier. Suicide is the leading cause of death for Australians aged between 15 and 49 and the second leading cause of death for those aged between 50 and 54.
With September being World Suicide Prevention month, Gold Coast Primary Health Network turns its focus on how it can support general practitioners to support the community. Three useful programs for GPs are:
Initial Assessment and Referral (IAR) Guidance and Decision support tool (DST)
This helps determine the most appropriate level of care for a person seeking mental health support, and offers a standardized, evidence-based approach to mental health care across the sector.
The IAR guidance identifies eight domains that should be considered when determining the next steps in the referral and treatment process for a person seeking mental health support. The information gathered is then used to recommend a service type and intensity (level of care) and inform a referral decision.
This process is based on a clinically informed algorithm and is calculated automatically using the digital Decision Support Tool (DST) which can be found at https://iar-dst.online.
Register your interest for local training in the IAR-DST by emailing iar-dst@gcphn.com.au. GPs can self-report to RACGP for CPD hours and are eligible for a $300 reimbursement.
Head to Health Phone Service
This free phone resource offers mental health service navigation for GPs and other health professionals looking to find appropriate mental health support for their patients.
The phone service can also be accessed by anyone of any age including children, young people, older adults, families, and carers. Calls are answered by an experienced team of mental health clinicians, who use the IAR-DST to make appropriate referral and support recommendations in collaboration with a patient’s preferences. They use their knowledge of the broad range of services available to identify the best option to suit an individual’s needs.
With the person’s consent, the intake team will keep GPs informed on the referral outcomes to support patient continuity of care.
Call 1800 595 212 Monday to Friday, 8:30am until 5pm (AEST), excluding public holidays.
GP Psychiatry Support Line
This is a free phone-in service exclusively for GPs to speak directly with a qualified psychiatrist to help manage the mental health care of your patients. It covers advice related to, but not limited to, diagnosis, medication, investigation, treatment pathways, and safety planning. After the call, receive a report of what was discussed including any psychiatry advice.
Call 1800 16 17 18 Monday to Friday, 7am until 7pm (AEST), excluding public holidays.
This article was distributed in the September/October 2023 edition of Doctor Magazine.
Gold Coast GPs can now directly refer into the Supporting Minds program, which provides free psychosocial services for people experiencing situational distress and people who identify as part of the LGBTIQAP+ community (aged 12-65 years) or, are gender questioning.
The Supporting Minds mental health service provides up to 3-months, moderate- intensity mental health support under two service streams:
The Supporting Minds model includes a brief mental health assessment, structured psychological interventions, and other structured interventions such as group-based lifestyle interventions.
The service model includes:
To refer into the Supporting Minds program:
If your patients require other mental health support, they can contact Head to Health on PH: 1800 595 212 where they can speak to a mental health professional and connect with a service that meets their needs. The Head to Health Phone Service provides information, advice and referrals to free and low-cost service in the area.
This article was distributed in the July/August 2023 edition of Doctor Magazine.
So we can provide you with the most accurate information,
please tell us a little more about yourself

